The Ultimate Runner’s Guide to Achilles Tendon Injuries
This is most likely an article you don’t want to read.
Here’s why:
Achilles tendon injuries can be stubborn, painful and depressing. If you’re reading this, then you likely have one. Luckily, we’re here to help.
This guide will explain why achilles tendon issues occur, and what you can do to limit the time it takes to heal it if you are suffering from achilles tendon aching, soreness, creaking or heel pain.
The Achilles tendon is the thickest and strongest tendon in your body, connecting your calf muscles to the back of your heel.
Virtually all of the force generated when you “toe off” the ground during running is transmitted by the Achilles, and this force can be as much as three times your body weight. And the faster you run, the more strain you put on the Achilles tendon.
As such, it’s prone to injury in many runners, but particularly those who do a lot of speed training, uphill running, or use a forefoot-striking style. Achilles tendon injuries account for 5-12% of all running injuries, and occur disproportionately in men.
This may be because of the faster absolute speeds men tend to train at, or may be due to other biomechanical factors.
Achilles tendonitis typically starts off as a dull stiffness in the tendon, which gradually goes away as the area gets warmed up. It may get worse with faster running, uphill running, or when wearing spikes and other low-heeled running shoes.
If you continue to train on it, the pain in the tendon will be more sharp and you will feel it more often, eventually impeding your ability even to jog lightly.
About two-thirds of Achilles tendonitis cases occur at the “midpoint” of the tendon, a few inches above the heel. The rest are mostly cases of “insertional” Achilles tendonitis, which occurs within an inch or so of the heelbone. Insertional Achilles tendonitis tends to be more difficult to get rid of, often because the bursa, a small fluid-filled sac right behind the tendon, can become irritated as well.
The common causes of Achilles tendonitis in runners
Here’s the deal:
The causes of Achilles tendonitis all appear to be related to excessive stress being transmitted through the tendon. Weak calf muscles, poor ankle range of motion, and excessive pronation have all been connected with the development of Achilles problems.The upshot is that all of these factors, plus training volume and so on, result in damage to the tendon.
While the term “tendonitis” implies that inflammation (-itis) is the root cause of the problem, in fact, the true cause is real, physical damage to the fibers of the Achilles tendon itself.
Much like a bungee cord is made up of tiny strands of rubber aligned together, tendons are comprised of small fiber-like proteins called collagen. Pain in the Achilles tendon is a result of damage to the collagen. Because of this, treatment options should start with ways to address this.
How can I treat my achilles tendon pain?
For a long time, researchers and doctors muddled about trying to address factors like calf strength & tightness, ankle range of motion, and pronation, assuming that the Achilles tendon would heal itself once these factors were corrected.
Unfortunately, it seems that the thick tendons of the body do not heal as rapidly or completely as we’d like.
The cause of this seems to be the collagen fibers:
When a tendon is damaged, collagen fibers are ruptured. The body is able to lay down new fibers to replace the damaged ones, but it does so in a rather disorganized way. The new collagen fibers look much like a mess of spaghetti when viewed on a microscope, in contrast to the smooth, aligned appearance that healthy tendon fibers have.
Unfortunately, it gets worse:
While we might propose that runners do calf stretching to loosen up their calf muscles and increase their ankle range of motion, this often does more harm than good—tugging aggressively on the damaged tendon fibers is much like pulling on either end of a knotted rope.
Instead, the main objective in treating Achilles tendon injuries should be healing the damaged tendon. The exercise of choice is the eccentric heel drop, which has an impressive research pedigree backing its use.
How does the eccentric heel drop help my achilles get better faster?
The strength protocol consists of two exercises: a straight-kneed and a bent-kneed eccentric heel drop.
The protocol calls for three sets of fifteen heel drops, both bent-kneed and straight-kneed, twice a day for twelve weeks.
Standing on a step with your ankles plantarflexed (at the top of a “calf raise”), shift all of your weight onto the injured leg.
Slowly use your calf muscles to lower your body down, dropping your heel beneath your forefoot. Use your uninjured leg to return to the “up” position.Do not use the injured side to get back to the “up” position!
The exercise is designed to cause some pain, and you are encouraged to continue doing it even with moderate discomfort. You should stop if the pain is excruciating, however.
Once you are able to do the heel drops without any pain, progressively add weight using a backpack. If you are unlucky enough to have Achilles tendon problems on both sides, use a step to help you get back to the “up” position, using your quads instead of your calves to return up.
What’s the bottom line?
The eccentric exercises are thought to selectively damage the Achilles tendon, stripping away the misaligned tendon fibers and allowing the body to lay down new fibers that are closer in alignment to the healthy collagen in the tendon.
This is why moderate pain during the exercises is a good thing, and why adding weight over time is necessary to progressively strengthen the tendon.
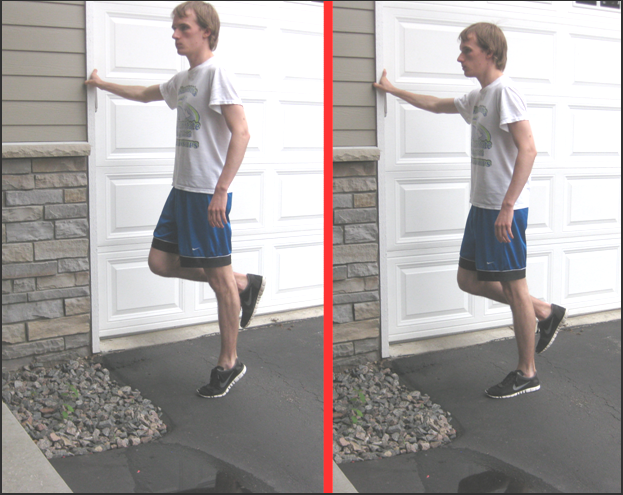
Exercise 1: The straight-knee eccentric heel drop.
In this picture, the injured side is the left leg. Note that the right leg is used to return to the “up” position. This exercise is one of two used in cases of midpoint Achilles tendonitis. Once you can perform this exercise pain-free, add resistance using weights in a backpack.
Exercise 2: The bent knee eccentric heel drop.
As with exercise 1, the opposite leg is used to return to the “up” position. This time, bend your leg at the knee and slowly lower yourself down. This is the second exercise for midpoint Achilles tendonitis. Add weight when you can do it pain free.
Exercise 3: Modifications for insertional Achilles tendonitis
Exercise 3: the flat-ground eccentric heel drop. This exercise is used for cases of insertional Achilles tendonitis, replacing exercises 1 & 2. Like the exercises for midpoint Achilles tendonitis, use the opposite leg to return to the “up” position and add weight once you can do it pain-free.
In the case of insertional Achilles tendonitis, the protocol is modified a bit: the exercise is done on flat ground, and only the straight-legged variant is done. All other aspects are identical (3×15 twice daily, adding weight, and so on).
Exclusive bonus: Download our full Achilles Injury Prevention Routine. It’s a PDF with images and descriptions of the 10 most effective prevention and rehab exercises for runners with Achilles issues.Download yours for free here.
Is there anything else I can do to speed healing?
While you are addressing the damage to the tendon fibers through eccentric heel drops, there are some steps you can take to help ameliorate some of the other contributing factors to your injury.
- While calf tightness and ankle range of motion are legitimate concerns, I still don’t think that aggressive calf stretching is an ideal solution, because of the tugging action on the tendon. Instead, try foam rolling your calves and applying a warm water bag to the muscle (but avoid heating the tendon!). Foam rolling your calf muscles can loosen them up without tugging too much on the Achilles tendon. Just make sure you are not making the 4 most common mistakes runners make when foam rolling.
- You can also stretch out your shins by leaning back in a kneeling stance to aid ankle range of motion.
- Footwear concerns should also be addressed at this point. If you have been wearing low-heeled “minimal” shoes, racing flats, or spikes, you ought to stick to more traditional shoes with a higher heel until your tendon is healthy again. Once you’ve healed up, you can gradually do some running in low-heeled shoes or even barefoot (on grass) to help accustom your Achilles to moving through its full range of motion. Poor casual footwear choices should not be overlooked too, especially for women. Some shoes can also put pressure on the back of your heel, irritating the insertion of the tendon. Generally, the closer a shoe is to looking and feeling like a “running shoe,” the better it is for your foot.
- Doctors and podiatrist may be keen to have you try out a custom orthotic to treat your Achilles problems. While it might be worth a shot, there isn’t a whole lot of scientific evidence backing their use in this case. Orthotics don’t reliably alter pronation, and even if they do, it’s uncertain as to whether this will increase or decrease stress on the Achilles.
Outline of treatment
Conservative treatments
These are cheap, easy to perform treatments that you can do it home in your own time. You should try to do as many of these as possible each day.
- Eccentric heel drops – 3 sets of 15 reps, twice per day for 12 weeks (if you only do one thing, do this!)
- Icing after each run
- Heating before each run with warm water or heating pack
- Contrast bath during the day – take two small buckets/trash cans and fill one with hot (hot bath temp) water and the other with ice water (cold enough so some ice still doesn’t melt) and put your whole leg (up to the calf) in the cold. Hold for 5 minutes and then switch to the hot for 5 minutes. Repeat 2 or 3 times, ending with cold. This helps rush blood in and out of the area, which facilitates healing
- Don’t take anti-inflammatory like Advil or ibuprofen. These stop the body’s natural healing agents and we want as much natural healing to occur as possible.
- Avoid excessive stretching – only very light, easy stretching until healed
- Massage your calves with a foam roller or The Stick.
- Heel lifts are a possible temporary solution. They restrict the Achilles’ range of motion, so can be helpful to get over the initial hump of the injury, but should be taken out after you are recovering.
- Switch to more supportive or traditional running shoes (higher heels) during your runs and while walking around until your pain is completely gone, and avoid flats and high heels!
- Ankle strengthening and mobility exercises.
- Sleep in a Strassburg sock or nightsplint to gently stretch the Achilles while sleeping.
Aggressive treatments
These treatments are a little more expensive or time consuming and are only suggested for if you suffer from chronic Achilles pain or the conservative treatments are not working for you.
- A custom orthotic might help alleviate the pain from excessive pronation. This is not a proven treatment, but for those runners who respond to orthotics, it can help.
- Iontophoresis with dexamathasone. This is a treatment offered by physical therapists that involves propelling anti-inflammatory steroids into the tendon. You need a prescription and a physical therapist to administer the treatment, but research has shown the potential to have a positive effect on the treatment of Achilles issues.
Strengthening and prevention
- Eccentric heel drops
- Ankle strengthening and mobility exercises
- Achilles rehab exercises
When can I return to running?
You can still run during this twelve-week period, but only if your Achilles does not flare up while doing so.
Use warm water to heat up the tendon before you run, and apply ice afterwards, even once you’ve started feeling better. Using a foam roller and hot water packs to loosen up your calves in the morning and at night is also not a bad idea, and don’t forget to take a look at what you’re wearing in your daily life.
If you have insertional Achilles tendonitis, use the modified flat eccentric heel drop exercise instead of the two variants off a step.
A custom orthotic or heel lift may be helpful, but should not be a first-line treatment option.